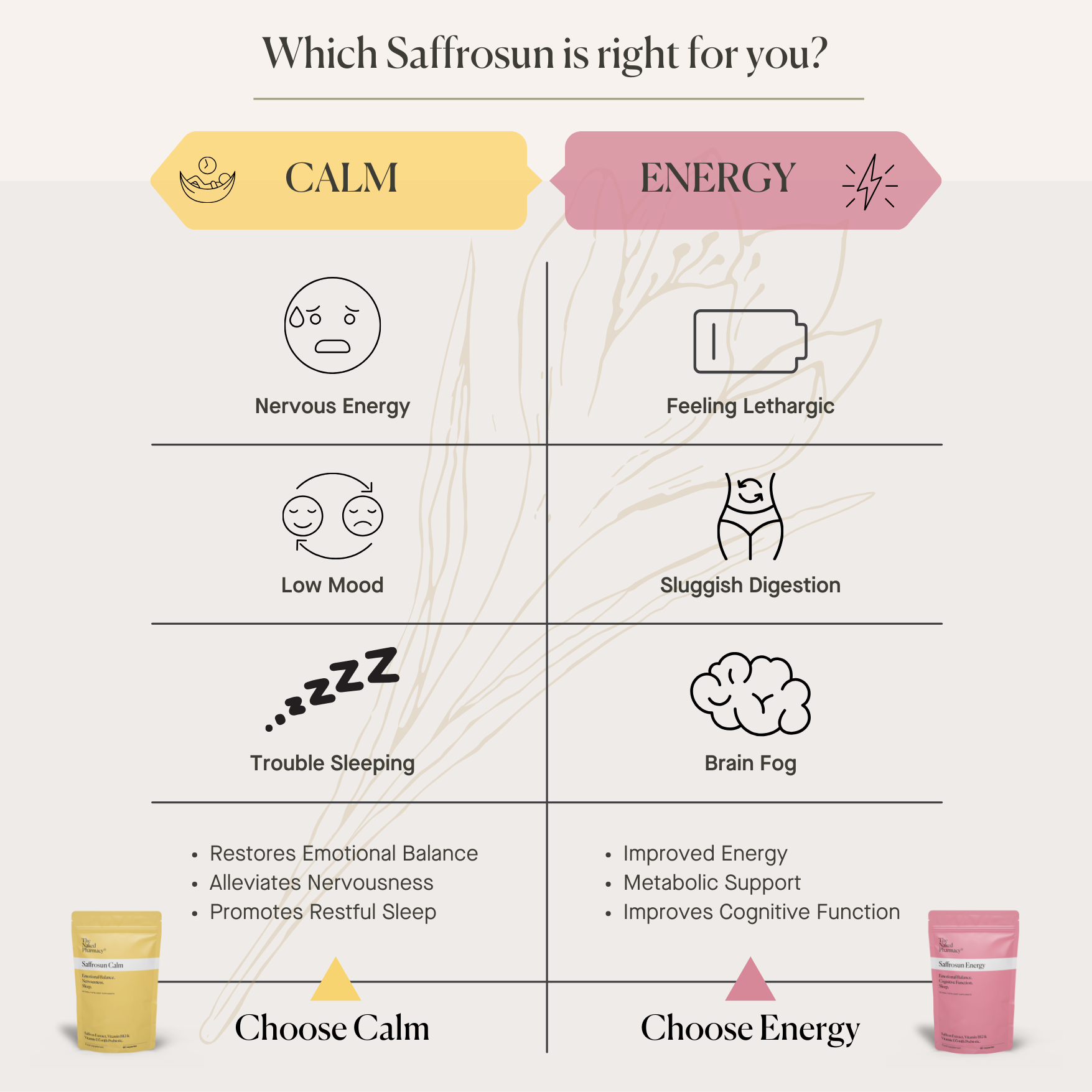
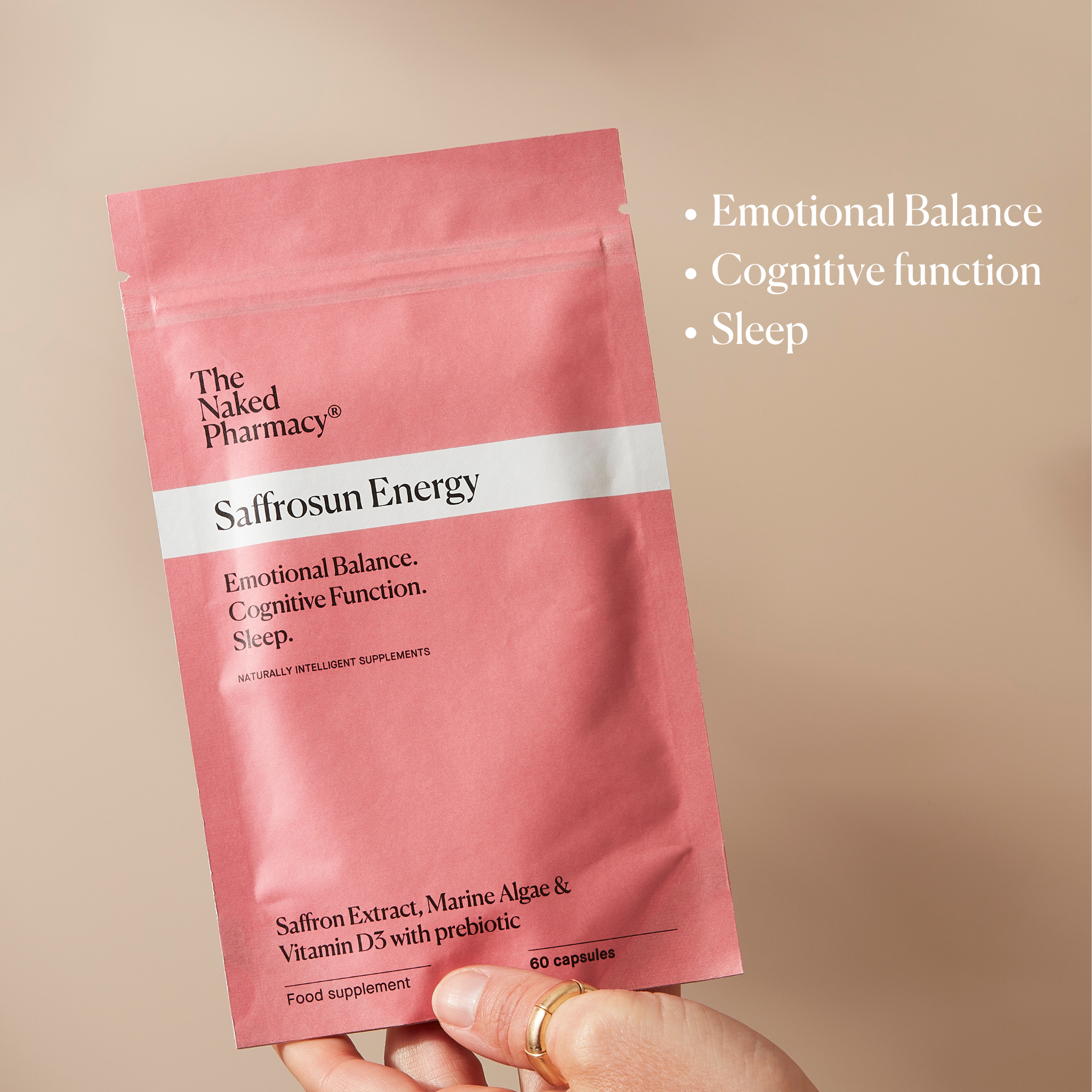
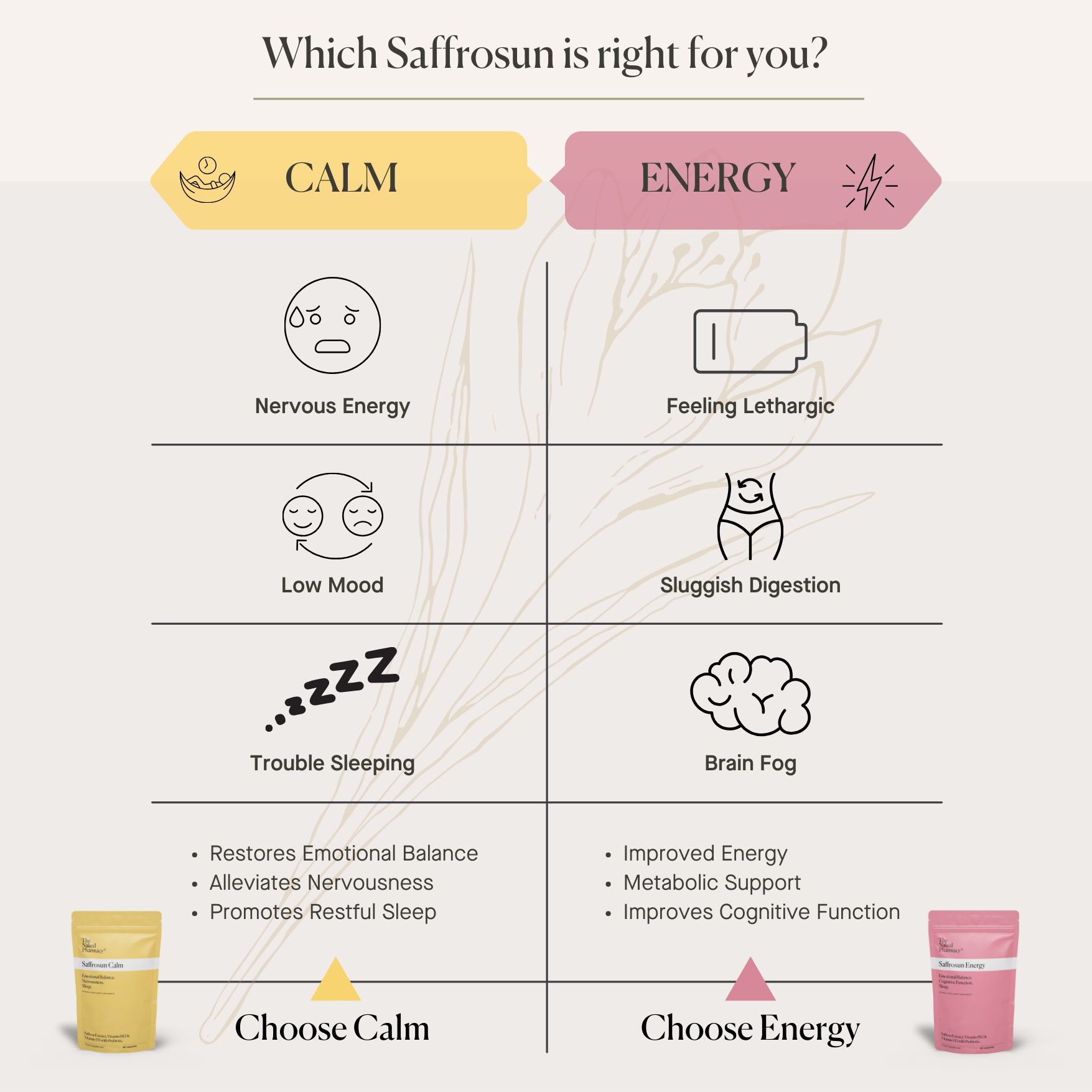
Shop our collection of pharmacist-formulated, evidence-backed natural supplements designed to support your well-being.
Discover our pharmacy services — book a consultation, free health advice and prescription only medication options.
What Our Customers Say
Why Choose Naked?
People
People are at the heart of what we do. Our pharmacists love to connect, offering free, advice to help you feel your best, naturally.
Purity
There's nothing to hide. No synthetics, no fillers, just pure, natural ingredients with potent bioactives for maximum benefit and absorption.
Proven
Our premium grade supplements are clinically tested to pharmaceutical standards for quality, strength and proven results.
Save 25% on The Naked Pharmacy Range
Receive regular scheduled deliveries
Skip, amend or cancel anytime

Online Health Assessment
Our team of qualified Pharmacists have designed this health assessment to help you understand your health needs better so we can provide you with personalised recommendations.
It only takes 2 minutes and you will instantly receive your personalised health solution.